Healthcare professionals and New School students share insight on how eating disorder treatment can become more inclusive for BIPOC and individuals in larger bodies.
Content warning: This article contains discussions of eating disorders and disordered behavior that may be triggering to those living with or in recovery from eating disorders.
When Brianna Theus, 26, opened an outpatient eating disorder center in Connecticut, she knew that she wanted it to serve people who had been left behind: Black, Indigenous, and people of color, men and those in larger bodies.
“I feel the need to really make sure that I create a space for people who feel like they don’t belong in treatment,” Theus said in a phone call to The New School Free Press. She explained that because she is Black herself, her patients feel that she can better understand what they are going through. “For some people, a lot of the time, they may struggle with growing up in a household that doesn’t believe in mental health. Or, they struggle, in a household where, maybe health isn’t always the first priority, which is something I can relate to.” Theus also said that she can relate to the food her patients grew up eating, which she says makes it a safer space.
She opened the center, called The Celestial Life, in 2016 after graduating from The University of Saint Joseph with a Bachelor of Science in Nutrition and Dietetics. Theus began working in eating disorder treatment centers during her time in school, where she attempted to rekindle clients’ healthy relationships with food.
Since opening The Celestial Life, Theus said, several of her clients have told her that they were either disregarded or misdiagnosed by doctors.
Black women and girls are less likely to be diagnosed with an eating disorder compared to their white counterparts, even though they are 50% more likely to suffer from bulimia nervosa, according to the National Eating Disorder Association. NEDA collected information from various sources about white and BIPOC women’s disordered eating behaviors. Clinicians identified 44% of white women’s eating behaviors as troublesome, along with 41% of Hispanic women and 17% of Black women who exhibited the same behavior.
“It comes from racism, and it also comes from fatphobia,” she said.
Unlike the healthcare system, eating disorders do not discriminate. Roughly 30 million Americans have struggled with an eating disorder throughout their lifetime, as reported by U.S. News. There are eight eating disorders specified in the DSM-5, a diagnostic manual published by the American Psychiatric Association, including anorexia nervosa, avoidant restrictive food disorder, binge eating disorder, bulimia nervosa, and orthorexia. According to the National Association of Anorexia Nervosa and Associated Disorders, eating disorders are the deadliest mental illness, followed by opioid overdose. A 2019 study by the University of California San Francisco found that only 21% of individuals recovering from anorexia will fully recover.
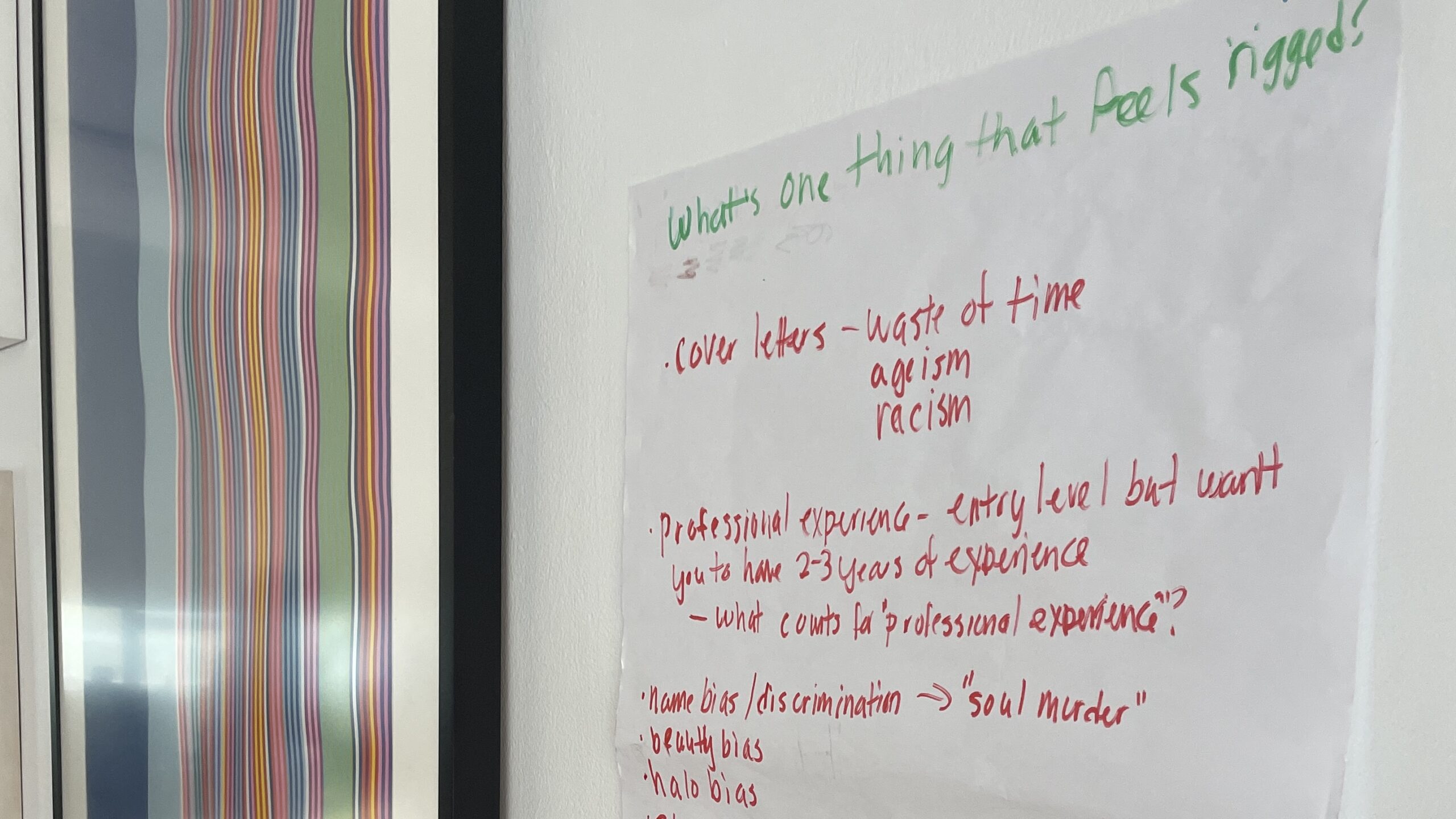
Several New School students have personally experienced such bias within the healthcare system.
Anya Rajagopal, a BIPOC second-year student at Eugene Lang College of Liberal Arts, felt that their access to treatment was delayed because they did not fulfill the stereotype of an eating disorder patient.
“I wasn’t their ideal vision, I guess, of someone with an eating disorder,” they said in a phone call with the Free Press. “It was bad in my eyes and my friends’ eyes. But to them, unless you’re emaciated and dying, you’re fine.”
Rajagopal said that their medical providers’ distorted perception of someone with an eating disorder impacted their view of the severity of their disorder.
“When they found out that I’m mixed, they would be like, ‘Oh, now this makes sense because you’re not fully Indian,’” they said. “But, if I had two Indian parents it would be like ‘Indian parents don’t care about mental health.’ So, I guess I am thankful in that sense that I am mixed because that’s really messed up.”
Ian Clifton, who volunteers with FEDUP, a virtual collective attempting to combat eating disorders amongst transgender and gender diverse individuals, is aware of the biases healthcare officials have against patients like Rajagopal. He himself believes that as a Black trans man, he was discriminated against by healthcare professionals, as it took him seven to eight years to be diagnosed. He has worked for FEDUP as a peer support educator for over four months, monitoring support groups for trans people with eating disorders. The experience of being invalidated by doctors is often brought up.
“There’s a stigma that only white, cisgender, females get eating disorders,” he said in a phone call with the Free Press.
Discrimination is not solely seen in the case of diagnosis. Some said they feel victimized in treatment centers.
“Most of the staff and most of the people who put together these treatment centers and the organizations are not BIPOC,” Theus said. “So, because of that, the face of eating disorders has typically been thin, white, young, cisgender [and] female. That is why a lot of the time BIPOC will not get treatment for eating disorders … When they get into treatment, it’s mostly white people. So, they don’t see themselves when they’re actually in treatment either.”
A Lang second-year student who asked to remain anonymous due to ongoing mental health struggles, initially questioned the validity of her eating disorder because she did not fit the mold of a “young, very thin, underweight, pale white girl.”
“I didn’t think for a long time that I had an eating disorder, even though I did, just because I wasn’t super underweight,” she said in a phone call with the Free Press. When her disorder was at its worst, she was not only told that she did not have a problem because she fit into a “normal” weight bracket, she was also frequently complimented by friends and teachers.
According to a study published in the Journal of General Internal Medicine, larger-bodied individuals are more likely to develop unhealthy weight control practices compared to those classified as “normal weight” or “underweight” people. Over 29% of the surveyors in an “overweight or obese” weight category displayed disordered eating behaviors, such as restricting, binging or purging, compared to 15.8% percent of surveyors in the “normal” weight category. Conversely, people with larger bodies are half as likely to receive an eating disorder diagnosis, compared to their thinner counterparts.
“I think to help better ensure that cases don’t fall through the cracks, [doctors should] alter how they go about giving diagnoses for eating disorders,” Brown said. “I think even though there is some change being made, a lot of healthcare professionals — even if they don’t think they do — have an implicit bias surrounding what an eating disorder patient looks like.”
Theus says she is doing what she can to help BIPOC and larger bodied people seek treatment. Her passion for nutrition and overall love for her job makes change easy, she said.
“I’m really able to listen to [my clients’] concerns and understand what is going on for them,” Theus said. “I’m able to understand more of where they’re coming from. I feel like [this] makes it a safer space for them.”
If you or someone you know is struggling with an eating disorder, call the Eating Disorders Association (NEDA) helpline at 800-931-2237.
A version of this article appeared in the Spring 2022 International Issue of The New School Free Press. Read more stories from the print issue here.






Leave a Reply